Remote Appearances
Telephonic and video conferencing are reported to slash spending. What are some of the options being offered?
Read More
How can we tackle it head-on?
Read More

This is a privately owned informational website that is not owned or operated by any state government agency.
If you have any questions about this domain name or website, please contact us here.
Visit The official United States Courts website
Courts today serve as the backbone of the justice system in many countries around the world. They are responsible for interpreting and applying the law to various disputes, ensuring that individuals and organizations are held accountable for their actions, and protecting the rights and liberties of citizens.
Modern courts can be divided into several categories based on their jurisdiction and the types of cases they handle:
Courts today are also increasingly adopting technology to improve efficiency and accessibility. Online filing systems, electronic document management, and video conferencing for remote hearings are just some examples of how courts are leveraging technology to streamline their operations and better serve the public.
Additionally, alternative dispute resolution (ADR) methods, such as mediation and arbitration, are becoming more popular as they offer a less formal and often faster way to resolve disputes compared to traditional court proceedings. Many courts now offer or even require parties to attempt ADR before proceeding to trial.
Another significant issue facing courts today is the need to address systemic inequalities and biases that may impact the fairness and impartiality of the justice system. Initiatives such as implicit bias training for judges, jury reform, and increased access to legal representation for low-income individuals are just some examples of how courts are working to address these challenges.
The United States courts system is a complex, multi-layered structure consisting of federal and state courts, each with its distinct jurisdiction and responsibilities. This hierarchical structure ensures the fair and efficient administration of justice in the United States.
Federal courts have jurisdiction over cases involving federal laws, disputes between states, and matters involving the United States government or its agencies. Federal courts are organized into three main levels:
State courts handle the majority of legal cases in the United States, including criminal matters, family law, probate, and most civil disputes. Each state has its own court system, which may vary in structure and organization, but generally follows a similar hierarchy:
Trial courts: Also known as lower courts or district courts, these are the entry point for most state cases. They handle both civil and criminal cases and may have specialized divisions for family law, probate, or small claims.
Intermediate appellate courts: Many states have an intermediate appellate court, typically called the Court of Appeals, which hears appeals from the trial courts. These courts review lower court decisions for errors in the application of the law or procedural issues.
State supreme courts: Each state has a supreme court, which serves as the highest court within the state's jurisdiction. State supreme courts hear appeals from intermediate appellate courts and have the final say on matters of state law.

Telephonic and video conferencing are reported to slash spending. What are some of the options being offered?
Read More
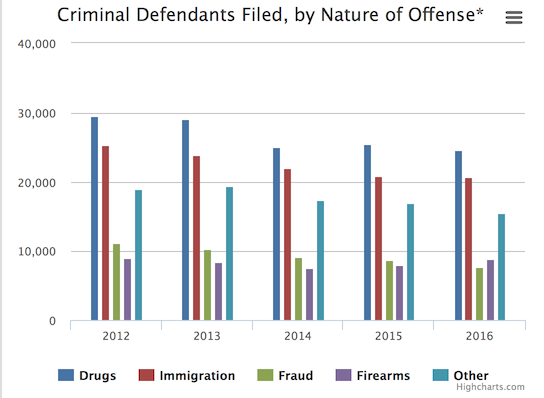
How is it impacting your court?
Read More




Get Social With Us